AUSTIN, Texas — Travis County health leaders say there are new concerns that contact tracing is not working in our current environment – that we need to find a better way to contain these outbreaks.
Getting back to business makes contact tracing more difficult.
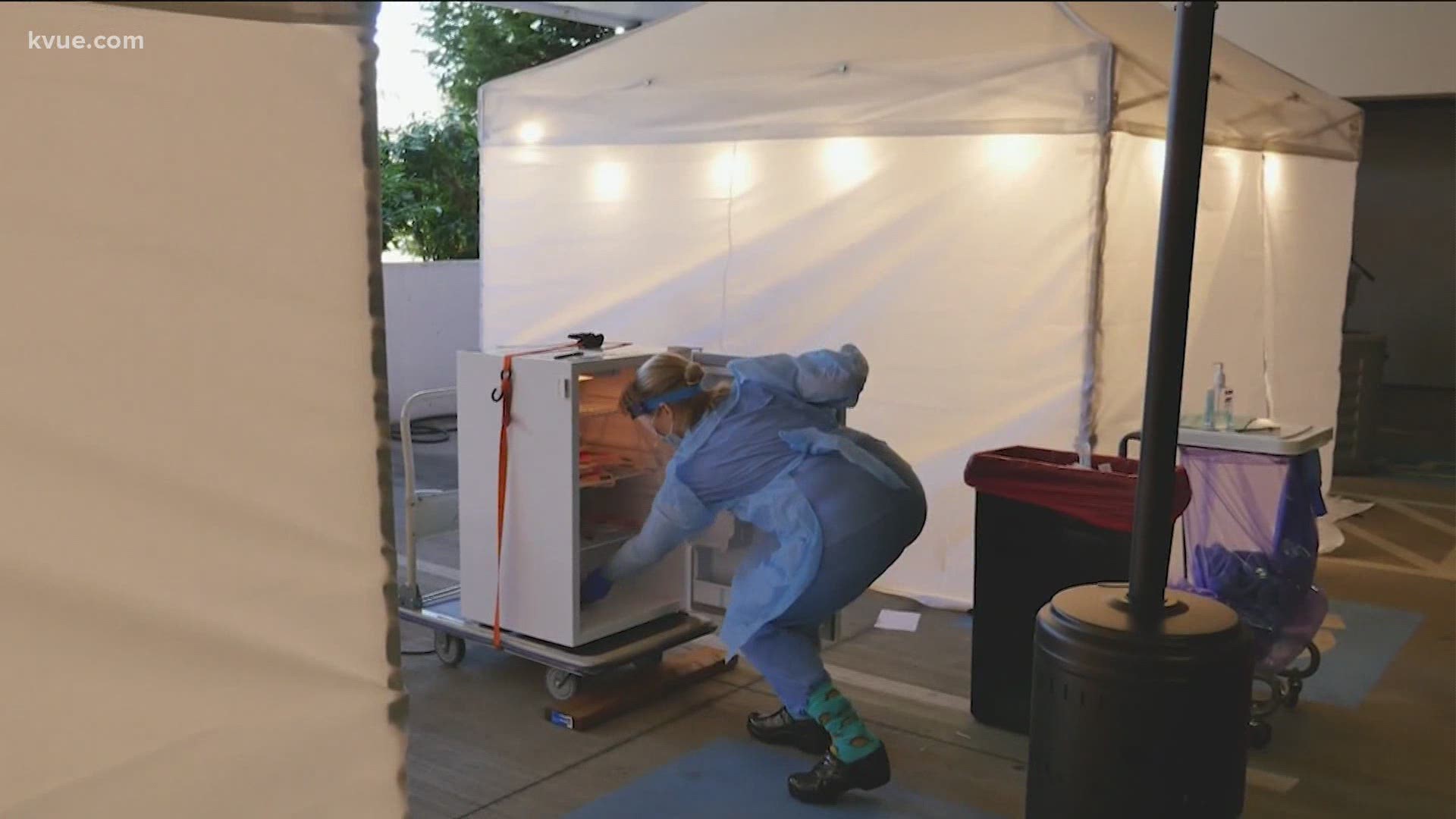
Dr. Darlene Bhavnani, Ph.D, is an infectious disease epidemiologist at the University of Texas' Dell Medical School helping track COVID-19 patients for months.
"I think there are a couple of factors at play. So, for contact tracing to be effective, it needs to be both timely and comprehensive. And I think what we're facing right now are challenges related to both in terms of timeliness,” said Bhavnani.
Here's how it's supposed to work: When someone tests positive for COVID-19, you isolate them and then track down everyone they've been in contact with. You then get those people tested and into quarantine.
RELATED: Abbott: Texas facing 'massive outbreak' as state sets another record for new cases in a single day
Tracking where people have been and who they may have come in contact with is more complicated with people not isolated at home.
Dr. Mark Escott told Travis County commissioners this week that most cases across the state are being reported by fax, not electronically.
“Unfortunately, still in public health here and across the state and across the country, this is a very manual and archaic process of getting information out and we're struggling with that,” he said.
“We need to move to a more electronic and efficient system that doesn't necessarily rely on paper processes for manual processes. So the more we can streamline our reporting, the more we can streamline and automate our internal processes, the quicker we'll be able to react,” said Bhavnani.
The increased caseload is another concern.
Think of it like traffic: At the beginning of the crisis, our roads were pretty empty. Now, things are picking back up. With hundreds, sometimes thousands, of new cases coming in every day, the process takes longer – sometimes 10 to 14 days to contact people who may be at risk.
“We're getting information from jurisdictions all across the state that say they cannot simply contact trace for everybody ... we're struggling to get all the cases in the system so that we know there are cases, and we really have to rethink the strategy when it comes to how we're going to address this,” said Escott.
“I think going back to what all public health experts have been saying and what the science is showing, this physical distancing is really important,” said Bhavnani.
The challenge of life with coronavirus.
Dell Medical School said it has 100 volunteers trained and currently helping with their contact tracing efforts. They plan to add more soon and currently have 200 volunteers on a waiting list. If you are interested in volunteering, you can go here to search for opportunities.
The team at UT Dell Medical School used contact tracing early on in the COVID-19 crisis after learning that three students had tested positive for the virus.
"It was a Saturday night. We all wanted to go home. And she said, 'I think they took a flight.' And so I said, ‘Well, we have to get on this and we need to follow up. We need to figure out the flight.’ We got on the phone with the tour company and they were helpful and shared information with us. We worked with Austin Public Health very closely to share the information and we were able to get flight manifests, which helped us track down the students," said Bhavnani.
Ultimately, 64 students tested positive. Sixty of those were connected to a spring break trip to Cabo San Lucas, Mexico.
Here’s how that contact tracing process worked with the UT students:
"We get on the phone with the person who has tested positive as soon as we can," she said. "And we interview them about when they might have started feeling bad. We try to understand their first day of symptoms. And that's extremely important because it tells us when they might have been infectious. We walk back two days from that date of symptom onset and walk forward 10 days and we try to understand who they may have exposed within that infectious period. Once we gather the names and numbers of their contacts, we are able to then have a team of people to follow up, call those contacts, make sure they're feeling OK, provide some education about what the next steps are regarding quarantine and isolation, and also potentially move them into our testing, looking out for testing.”
PEOPLE ARE ALSO READING: